About Acute Kidney Injury (AKI)
Acute Kidney Injury (AKI) is a clinical condition characterised by a sudden decrease in kidney function, leading to the accumulation of urea and other nitrogenous waste products, as well as metabolic abnormalities such as dysregulation of extracellular volume and electrolytes.
In patients under 18, stage 3 AKI is additionally defined by the Kidney Disease: Improving Global Outcomes (KDIGO) as a decline in estimated glomerular filtration rate (eGFR) to less than 35 mL/min/1.73 m2.
The Kidney Disease: Improving Global Outcomes (KDIGO) defines Acute Kidney Injury (AKI) based on the following criteria:
- An increase in serum creatinine by ≥0.3 mg/dL within 48 hours, or
- An increase in serum creatinine to ≥1.5 times the baseline value within the prior seven days, or
- A reduction in urine volume to less than 0.5 mL/kg/hour for six hours.
Causes of AKI
There are 3 subcategories of causes of acute kidney injury, which are below:
Prerenal causes
- Hypovolemia: Acute diarrhoea, vomiting, burn, sepsis, haemorrhage, diabetic ketoacidosis
- Congestive heart failure
- Perinatal asphyxia
- Third space loss: septicemia, nephrotic syndrome
- Drugs: Diuretics, ACE inhibitors
Renal/intrinsic causes
- Vascular: HUS, Vasculitis, renal vein thrombosis
- Tubular
- Acute tubular necrosis (ATN)
- Wasp sting, snake venom
- Nephrotoxic drugs, e.g. diethyl glycol, methanol
- Tumor lysis syndrome (uric acid crystals tubular obstruction)
- Glomerulonephritis
- Post-infectious GN
- Membranous proliferative GN
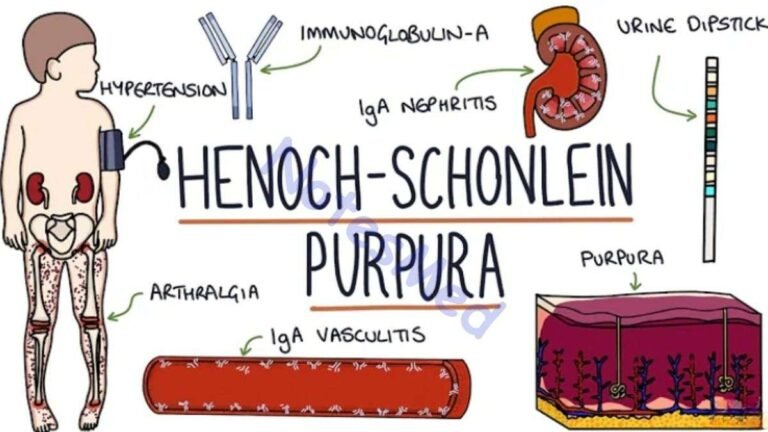
- Systemic disorder: SLE, Henoch-Schonlein syndrome, Microscopic polyangiitis
- Interstitial: Interstitial nephritis, pyelonephritis
- Medications: aminoglycosides, radiocontrast, amphotericin B, ACE inhibitor, Indomethacin, NSAIDs
Post-renal causes
- Urinary obstruction:
- Posterior urethral valves, Urethral stricture
- Bilateral UPJ obstruction
- Blood clot in the urinary tract
- Neurogenic bladder
Pathogenesis
- A rapid decline in GFR, which results in
- Accumulation of nitrogenous wastes in the body
- Elevation of blood urea, creatinine, blood urea nitrogen (BUN)
- Impairment of water, electrolytes, and acid-base balances
- Dyselectrolytaemia e.g. hyperkalemia
- Acid-base imbalance, e.g. metabolic acidosis
- Fluid overload, hypertension
- Accumulation of nitrogenous wastes in the body
Clinical features
There are the following clinical features;
Hallmark of Acute Kidney Injury:
- Scanty urine (oliguria)
- Complete cessation of urine (anuria)
Other manifestation
- Vomiting
- Convulsions
Approach to Acute Kidney Injury
History
- H/o anuria, oliguria, vomiting, or blood loss
- Assessment of fluid intake in the previous 24 hours
- History to find out the causes –
- Fluid loss, e.g. diarrhoea, severe vomiting
- Pre-existing kidney disease, e.g. AGN, NS
- Ingestion of nephrotoxic drugs e.g. diethyl glycol in paracetamol, aminoglycoside
Examination
- Facial puffiness, oedema, and hypertension
- Heart failure (hepatomegaly, pulmonary oedema)
- Toxic features of acute kidney injury, e.g. unconsciousness, arrhythmia, vomiting, convulsion
- Flank: Palpable renal mass (renal vein thrombosis)
- Urinary bladder: Palpable ( PUV)
- Hemodynamic status e.g. pulse, BP, capillary refill time
Investigation
- CBC: Hb (reduced), Leukopenia (sepsis), Thrombocytopenia (HUS)
- Blood biochemistry
- S creatinine, urea, BUN: Raised
- S electrolytes: High K+, low HCO3–, Low Na+
- S calcium (low), Phosphate (high)
- ABG: Metabolic acidosis
- Urine R/M/E: RBC, protein, crystal, granular cast
- Blood: ASO titre, C3, C4, ANA, Anti-ds DNA, Ab to GBM
- Chest X-Ray: Cardiomegaly, pulmonary congestion, pleural effusion
- Renal ultrasound scan: To rule out UTI obstruction and Kidney morphology
- Renal biopsy
- ECG
Treatment
- Hospitalise the child.
- Counsel the parents about the illness.
- Discontinue nephrotoxic drugs if any.
- Introduce, a catheter when suspected PUV, and
- Monitor urine output.
Treatment is always supportive and then others
- Fluid resuscitation
- Treatment of the underlying cause of AKI
- Management of associated conditions
- Nutrition support
- Dialysis
- Renal Replacement Therapy
Fluid resuscitation
- No volume overload or CCF
- Normal saline, 20 mL/kg over 30 minutes (hypovolemic patient generally voids within 2 hours
- Hypotension due to sepsis
- IV fluid, along with continuous infusion of vasopressor
- Adequate circulatory volume is established/pulmonary oedema
- O2 inhalation, propped-up position
- Furosemide (2-4 mg/kg)- single IV
- No urine output with this single dose of frusemide
- Continuous diuretic infusion ± Injection Dopamine (2-3 g/kg/min) for renal cortical blood flow
- If still no response to the diuretic challenge
- Stop giving diuretics
- Restrict fluid to 400 mL/m2 /day (insensible loss) + previous day urine output
- Replace any external loss (blood, GIT) meticulously with appropriate fluid
- Readjust fluid allocation if volume overload
- Monitor intake, output, body weight, and serum chemistries daily
Management of associated conditions
Hyperkalemia
- Calcium gluconate 10% IV 0.5-1 ml/kg over 5-10 minutes
- Salbutamol 5-10 mg nebulized
- Sodium bicarbonate 7.5% 1-2 ml/kg over 15 minutes
- Dextrose 10% 0.5-1 g/kg and insulin 0.1-0.2 U/kg IV
- Calcium or sodium resonium (Kayexalate) 1 g/kg/day
Metabolic acidosis:
- Sodium bicarbonate (1ml/kg), IV if less than 18 mEq/l
Hypertension
- Asymptomatic cases: Isradipine (0.05-0.15 mg/kg/dose) QID, nifedipine
- Symptomatic cases e.g. hypertensive encephalopathy, Na Nitroprusside (0.5-10 μg/kg/min) or Labetalol (0.25-3.0 mg/kg/hour) by infusion under the supervision
- Others: Amlodipine ( 0.1-0.6 mg/kg/day) BID
- Labetelol (4-40 mg/kg/day)
Nutritional support
- Encourage a high-calorie diet, rich in carbohydrates and fat, to reduce protein catabolism
- Protein: 1-1.2 g/kg in infants, 0.8-1.2 g/kg in others
- Calories: 60-80 cal/kg/day
- Vitamin and micronutrient supplements
- Restrict extra salt intake
- Avoid foods rich in potassium, e.g. citrus fruits, tomato paste, chocolates, and potato chips