What is meningitis?
Meningitis is an inflammation of the leptomeninges & CSF within the subarachnoid space of the brain and spinal cord which covered it. In meningitis, there is an enlargement of the meninges in your brain or spinal cord.
The meninges are the 3 membrane layers include the dura mater, arachnoid mater, & pia mater that cover the brain & spinal cord body. Meningitis can occur when fluid (CSF) surrounding the meninges layer becomes infected.
There are various types of meningitis present some common types of meningitis we can discuss briefly.
Some common clinical features
- Fever, Headache, Meningism
- Signs of cerebral dysfunction such as confusion, delirium, or decreasing level of consciousness ranging from lethargy to coma.
- Photophobia
- Kernig’s sign
- Brudzinski’s sign is the physical examination symptoms of meningitis, In this situation, patients have severe neck stiffness that causes a patient’s hips and knees to flex when the neck is flexed.
Types of meningitis
- Pyogenic/purulent meningitis (Acute bacterial meningitis) is an infection of the meninges associated with a marked, acute inflammatory exudate and is usually caused by a bacterial infection in the covering.
- Chronic meningitis has a more insidious or dishonest onset with the progression of signs and symptoms over a period of weeks. It is usually associated with mycobacteria or fungi that produce granulomatous inflammatory changes and occasionally associated with protozoal agents.
- Aseptic meningitis is a syndrome of meningeal inflammation associated mostly with an increase in lymphocyte and other mononuclear cells in the CSF and the absence of readily cultivable bacteria or fungi. It is most commonly associated with viral infections and is often self-limiting.
Causes of meningitis
There are mainly two types of causes are present such as infection (mainly) and chemical agents. There are some infectious agents are shown in below
- Common bacterial agents:
- Streptococcus pneumoniae
- N. meningitidis
- H. influenzae
- Group B Streptococcus or Streptococcus agalactiae
- Listeria monocytogenes
- Staphylococcus aureus and CoNS
- Viruses:
- Enterovirus
- Mumps
- Lymphocytic choriomeningitis
- Epstein–Barr virus (EBV)
- Herpes simplex virus
- human immunodeficiency viruses (HIV)
- Arbovirus, etc
- Fungi:
- Candida albicans
- Cryptococcus neoformans
- Parasites:
- Toxoplasma gondii
- Naegleria fowlerii
- Acanthamoeba
- Taenia solium
Route of transmission
- Hematogenous: It is the most common route of transmission meningitis.
- From adjacent organs: Sinusitis, Chronic Suppurative Otitis Media, mastoiditis, osteomyelitis of skull bones.
- Direct Implantation: Iatrogenic during surgery, lumbar puncture, and Road traffic accidents.
Laboratory diagnosis of meningitis
The specimen is CSF taken by Lumbar puncture (spinal tap) needle method done on the lower back at the site of the lumbar region at the level between L3-L4 vertebrae. It should be examined immediately after collection or placed in the incubator for examination within an hour. Fluid in three separate vials: 1 each for cell count, chemical examination, and microbiological study.
Findings of CSF analysis: Normal Vs Various Infections
| Clinical condition | Cell count (total/mm3) | Type of cell | Glucose(mg/dL) | Protein(mm g/dL) |
| Normal | 0-3 | lymphocytes | 40-80 | 30-45 |
| Ac.pyogenic meningitis | 500-10000 | Neutrophil 95%, lymphocytes 5% | Diminished or absent (10-20) | Highly increased (100-160) |
| Viral meningitis | 4-10 | lymphocytes | normal | Slightly increased (60-80) |
| Tuberculosis/Fungal infection | 50-500 | Neutrophil 10%, lymphocytes 90% | Diminished (30-50) | Slightly increased (80-120) |
Acute pyogenic meningitis
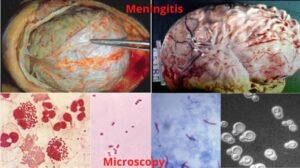
- Microscopy:
- Gram stain of centrifuged deposit shows sufficient pus cells and few Gram-positive or Gram-negative organisms.
- In inflammatory conditions, meningeal vessels are engorged and prominent and the tract of pus may extend along blood vessels.
- Chemical analysis: diminished glucose and increased protein levels.
- Culture:
- Centrifuged deposit of CSF is inoculated onto blood agar, chocolate agar, and cooked meat broth, incubated in an atmosphere of 5-10% of CO2, isolated organisms are identified by biochemical or serological tests.
- Blood culture: useful and about 50% positive in N.meningitidis, H.influenzae, and S.pneumoniae.
- Demonstration of bacterial products:
- The bacterial antigen can be detected or diagnosed by;
- Latex agglutination
- Counter-current immunoelectrophoresis (CIEP)
- ELISA
- By using specific antisera to the common serogroups of N.meningitidis, H.influenzae, and S.pneumoniae
- The bacterial antigen can be detected or diagnosed by;
- Bacterial endotoxin: Limulus lysate test.
Tuberculous meningitis
- Specimen is CSF
- Microscopy: Ziehl-Neelsen staining of the smear that prepared from centrifuged deposit shows a fair number of lymphocytes along with few acid-fast bacilli
- Culture: centrifuged deposit of CSF that inoculated on Lowenstein-Jensen(LJ) media & incubated at 37 ̊C for 6 to 8 weeks
Aseptic meningitis
- The specimen is CSF collection, and cell count and biochemical analysis are mentions above.
- Microscopy, culture, and another test may be performed according to the suspected causative agent (viruses, fungi, or protozoa)
- Amoebas: mixed sediment as a wet preparation under phase-contrast microscopy and stain by India ink stain, for example, is Cryptococcus neoformans.
Direct detection of the etiologic agent
- Antigen: Reagents & complete systems for the rapid detection of antigen is CSF are available in this case.
- Bacteria: rapid antigen detection from CSF by latex agglutination and co-agglutination ( use antibody-coated particle that will bind to a specific antigen, resulting in macroscopically visible agglutination.
- These reagents should be used as an adjunct to standard methods or procedures.
- There are various diagnostic tests are available some tests are mention above and some common diagnosis of meningitis starts with a take a health history and start to physical examination. During the physical examination, there should be a check following fever, heart rate increased, neck stiffness, loss of consciousness, etc.
- Common diagnosis tests are
- Blood culture
- Complete blood cell count
- Chest X-ray: for presence or absence of pneumonia, tuberculosis, or fungal infections.
- CT scan: for brain abscess or sinusitis
Complications
There are various complications associated with meningitis some complications are
- Seizures
- Hearing loss
- Vision loss
- Memory loss
- Arthritis
- Migraine headaches
- Hydrocephalus
- Subdural empyema
Management of meningitis
- In bacterial meningitis patients requires immediate hospitalization and early diagnosis and treatment will prevent brain damage and death. It is treated with intravenous antibiotics but there’s no specific antibiotic for bacterial meningitis but It depends on the bacterial infection involvement.
- Fungal meningitis is treated with various antifungal agents.
- Parasitic meningitis may either involve treating just the symptoms presenting or attempting to treat the infection directly & depending on the cause, this type may get better without antibiotic treatment.
- Viral meningitis may resolve on its own, but some causative agents of viral meningitis will be treated with intravenous antiviral drugs.
Preventions
- Adequate amount of rest
- Stop smoking
- Avoid contact with a sick person.
- Vaccination should be done some infections, for example, Haemophilus infeuenzae type B (Hib) vaccine, meningococcal vaccine, etc are found in the medical center.
- Regular exercise and maintains personal hygiene.