Bronchial asthma is a chronic inflammatory condition of the respiratory tract characterized by episodic exacerbations of hyperresponsiveness and reversible airway obstruction.
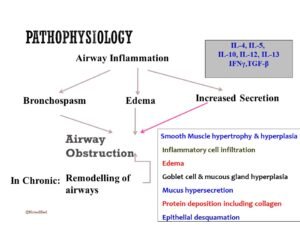
Pathophysiology
The early phase of bronchial asthma occurs within 15-30 minutes and is marked by bronchoconstriction, primarily due to the release of histamine, leukotrienes, and bradykinin. The late phase occurs after 4-12 hours and is characterized by airway inflammation and increased secretion.
Asthma triggers
Asthma triggers encompass a variety of factors:
- Allergens: including house dust mites, mold, pollen, and certain drugs.
- Environmental factors: such as smoke, dust, strong odors/fumes, and exposure to cold air.
- Physical activity.
- Emotional triggers.
Clinical features
Symptoms
- Intermittent dry cough, recurrent or nocturnal episodic cough
- Wheezing (in acute exacerbation or advanced asthma)
- Breathlessness or shortness of breath
- Chest tightness (only expressed by older children)
- Nonspecific
- Fatigue
- Exercise intolerance.
- Poor sleep
General examination
- Dyspneic
- Prominent accessory muscles of respiration
- Air hunger, cyanosis
- Flaring of alae nasi
- Altered sensorium in acute exacerbations.
Examination of chest
- Inspection: Tachypnea, chest hyperinflated, presence of subcostal, suprasternal, and intercostal recessions
- Palpation: Reduced chest expansion but central trachea
- Percussion: hyper-resonant
- Auscultation: Vesicular breath sound with prolonged expiration, rhonchi present.
Differential Diagnosis
- Bronchiolitis
- GERD
- Hypersensitivity pneumonitis
- Foreign Body inhalation
- Cystic fibrosis
Diagnosis
Generally, diagnosis is based on clinical, but laboratory support has little role.
Clinical evidence
- Presenting complaints like recurrent cough, breathlessness, wheezing, etc.
- History of asthma
Laboratory Investigation
- PEFR: Morning-evening variation>20%
- Low FEV1
- FEV1/FVC<0.8
- Bronchodilator response (beta agonist): Improvement in FEV1≥12%
- Exercise challenge: Worsening in FEV1 ≥ 15%
- Chest X-ray: hyperinflation of lungs (low flat diaphragm and more horizontal ribs) and tubular heart
- Absolute Eosinophil Count (AEC) test: may be increased.
- Allergy test but limited role
Treatment
Goals
- Maintain normal activity.
- Prevent sleep disturbance.
- Prevent chronic asthma symptoms.
- Prevent severe exacerbation.
- Less or No side effects from drug therapy
Drugs
- Beta 2 agonist (inhaled): salbutamol, terbutaline
- Inhaled anticholinergics: Ipratropium bromide
- Short course systemic steroid: oral prednisolone, Methyl prednisolone.