What is bronchial asthma?
Bronchial asthma is a chronic inflammatory condition of the respiratory tract characterised by episodic exacerbations of hyperresponsiveness and reversible airway obstruction.
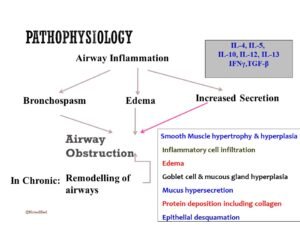
Pathophysiology
The early phase of bronchial asthma occurs within 15-30 minutes and is marked by bronchoconstriction, primarily due to the release of histamine, leukotrienes, and bradykinin. The late phase occurs after 4-12 hours and is characterised by airway inflammation and increased secretion.
Asthma triggers
Asthma triggers encompass a variety of factors:
- Allergens: including house dust mites, mould, pollen, and certain drugs.
- Environmental factors: smoke, dust, strong odours/fumes, and exposure to cold air.
- Physical activity.
- Emotional triggers.
Clinical features
Symptoms
- Intermittent dry cough, recurrent or nocturnal episodic cough
- Wheezing (in acute exacerbation or advanced asthma)
- Breathlessness or shortness of breath
- Chest tightness (only expressed by older children)
- Nonspecific
- Fatigue
- Exercise intolerance.
- Poor sleep
General examination
- Dyspneic
- Prominent accessory muscles of respiration
- Air hunger, cyanosis
- Flaring of alae nasi
- Altered sensorium in acute exacerbations.
Examination of the chest
- Inspection: Tachypnea, chest hyperinflated, presence of subcostal, suprasternal, and intercostal recessions, use of accessory respiratory muscles, and cyanosis.
- Palpation: Reduced chest expansion, but central trachea
- Percussion: hyper-resonant
- Auscultation: Vesicular breath sound with prolonged expiration, rhonchi present throughout the chest, more prominent during expiration than inspiration.
Differential Diagnosis
- Bronchiolitis
- GERD
- Hypersensitivity pneumonitis
- Foreign Body inhalation
- Cystic fibrosis
Diagnosis
Generally, diagnosis is based on clinical, but laboratory support has little role.
Clinical evidence
- Presenting complaints like recurrent cough, breathlessness, wheezing, etc.
- History of asthma
Laboratory Investigation
- Pulmonary function tests:
- Peak expiratory flow rate (PEFR): Durnal variation in PEF (the lowest values typically being recorded in the morning), more than 20% is considered diagnostic.
- Low FEV1
- FEV1/FVC<0.8
- Bronchodilator response (beta agonist): Improvement in FEV1≥12%
- Exercise challenge: Worsening in FEV1 ≥ 15%
- Chest X-ray:
- Usually normal findings.
- Acute asthma is accompanied by hyperinflation, and lobar collapse may be seen if mucus has occluded a large bronchus. X-ray of the chest shows a low, flat diaphragm and more horizontal ribs and a tubular heart.
- Measurement of allergic status:
- Sputum or peripheral blood eosinophil count may be elevated, and the serum total IgE is typically elevated in atopic asthma.
- Skin prick tests are simple and provide a rapid assessment of atopy.
- Measurement of allergen-specific IgE.
- Allergy test has but limited role.
- Assessment of airway inflammation: induced sputum and exhaled breath.
Treatment
Goals of Treatment
- Maintain normal activity.
- Prevent sleep disturbance.
- Prevent chronic asthma symptoms.
- Prevent severe exacerbation.
- Less or no side effects from drug therapy
Steps of treatment of bronchial asthma
- High concentration of oxygen
- High doses of inhaled bronchodilators:
- Beta 2 agonist (inhaled): salbutamol, terbutaline
- Inhaled anticholinergics: Ipratropium bromide
- Short course systemic steroid: oral prednisolone, Methyl prednisolone.
- Intravenous fluid: to correct dehydration.
- Subsequent management: if the condition is very severe:
- Intravenous aminophylline
- intravenous magnesium sulphate (MgSO4)
- Monitoring of treatment:
- PEFR should be recorded every 15-30 minutes and then every 4-6 hours
- Pulse oximetry should ensure that SpO2 remains more than 92%.
Step care management of bronchial asthma/chronic persistent asthma:
The step care management of bronchial asthma:
- Step up therapy:
- Step 1: Occasional use of inhaled short-acting β2-adrenoreceptor agonist bronchodilators.
- Step 2: Introduction of regular preventer therapy: inhaled corticosteroids
- Step 3: Add-on therapy: Long-acting inhaled β2-adrenoreceptor agonist or leukotriene receptor antagonist.
- Step 4: Poor control on moderate dose of inhaled steroid and add-on therapy: addition of a fourth drug.
- Step 5: Continuous or frequent use of oral steroids
- Step down therapy: Once asthma control is established, the dose of inhaled or oral corticosteroid should be titrated to the lowest dose at which effective control of asthma is maintained.
Criteria for discharging a patient with bronchial asthma
- The patient should be stable on oral medication.
- PEF>75% of predicted or personal best record.
- Nebulization should be discontinued 24 hours before discharge.
Status asthmaticus/acute severe asthma
The term acute severe asthma is used to mean an exacerbation of asthma that has not been controlled by the use of standard medication. Patients with acute severe asthma typically have:
- The inability to complete a sentence in one breath
- A respiratory rate of ≥25 breaths/min
- Tachycardia≥110 beats/min (pulsus paradoxus is not useful as it is only present in 45% of cases)
- PEFR 33-50% of predicted normal or best.
Life-threatening features of acute severe bronchial asthma
- PEF<33% predicted (<100 L/min)
- SpO2 <92% or PaO2 <8 kPa (60 mmHg) (especially if being treated with oxygen)
- Normal or raised PaCO2.
- Silent chest
- Cyanosis
- Feeble respiratory effort
- Hypotension
- Bradycardia or arrhythmias
- Exhaustion
- Confusion
- Coma
What are the indications for assisted ventilation in acute severe asthma?
There are the following indications for assisted ventilation in acute severe asthma:
- Coma
- Respiratory arrest
- Deterioration of arterial blood gas tensions despite optimal therapy:
- PaO2 <8 kPa (60 mmHg) and falling.
- PaCO2 >6 kPa (45 mmHg) and rising.
- pH low and falling (Hydrogen ion high and rising)
- Exhaustion, confusion, drowsiness.
What is cough variant asthma?
In some patients, cough is the predominant feature and has no wheeze or breathlessness; this is called cough variant asthma.
Using the instructions of the inhaler:
- Remove the cap and shake the inhaler.
- Breathe out gently and place the mouthpiece into your mouth.
- Incline the head backwards to minimise oropharyngeal deposition.
- Simultaneously, begin a slow, deep inspiration, depress the canister and continue to inhale.
- Hold your breath for 10 seconds.
- Rinse of the mouth with water.