What is Wound Healing?
Wound healing is a process of replacement of dead tissue by living tissue. If the supporting structures of the tissue are severely damaged and then repair occurs by the laying down of some connective (fibrous) tissue & this process may result in the formation of a scar.
Although the fibrous scar is not normal, it provides enough structural stability and that the injured tissue is usually able to function.
After Injury to cells and tissues, a series of events take place to initiate the process of healing. The wound healing process can be divided into 3 categories, they are;
- Regeneration
- Repair
- Fibrosis
What is Regeneration?
Regeneration refers to the proliferation of cells and tissues to replace the lost structure essentially returning to a normal state. It occurs due to the proliferation of cells that survive after injury and retain the capacity to proliferate.
Example: in the swiftly dividing epithelial cell present on the intestines and skin, and in some other parenchymal organs, like the liver. In some other cases, tissue stem cells may give to the restoration of damaged tissues.
But in the case of lower animals like salamanders and fish that regenerate entire limbs or appendages and mammals have a limited capacity to regenerate their damaged tissues or lost tissue and organs.
What is Repair?
In the repair stage, the replacement of damaged or lost tissue by granulation tissue that matures to form scar tissue. Repair occurs when the surrounding specialized cells do not possess any capacity to proliferate and replace the lost tissue or damaged tissue like in muscle and neurons. Regeneration occurs in labile cells & repair occurs in permanent cells.
What is Fibrosis?
Fibrosis is an extensive deposition of collagen that occurs due to persistent injury in the chronic inflammatory process or disease such as; cirrhosis of the liver, kidney, lungs, etc.
There are the following types of cells present on the basis of regeneration capacity, they are
- Labile cells ( continuously dividing types of cells)
- Quiescent (stable cells)
- Permanent cells(non-dividing types of cell)
- Labile cells (continuously dividing cells)
- These cells Proliferate throughout life replacing those tissues that are destroyed. E.g. Stratified squamous epithelium of the skin, oral cavity, vagina, cervix, the lining mucosa all excretory ducts of glands (salivary gland, pancreas, biliary tree, etc.).
- The squamous epithelial cell gives way to the columnar epithelium of the gastrointestinal tract.
- Transitional epithelium of urinary tract.
- Cells of bone marrow and hematopoietic tissues.
- Stable cells( Quiescent cells)
- Normally they have a low capacity of replication, however, can undergo rapid division in response to stimuli. e.g. parenchymal cells of the kidney, liver, and pancreas, etc.
- Mesenchymal cells such as smooth muscle cell and fibroblast
- Vascular endothelial cells with the exception of the liver, stable cells have limited capacity to regenerate after injury.
- Non-dividing (permanent cells)
- Actually, these types of cells have no capacity to proliferate. So regeneration occurs by scar formation. Example: Neurons, and cardiac muscle, skeletal muscle.
Steps in scar formation
- Angiogenesis: formation of new blood vessels(VEGF) from an existing one.
- Formation of granulation tissue:
- It is immature mesenchymal (connective) tissue with a proliferation of fibroblast with macrophages and the formation of new blood vessels.
- The term granulation tissues derive from its pink, soft, granular appearance on the surface of wounds.
- These tissues progressively invade the site of injury & the number of granulation tissue that is formed depends on the size of the tissue deficit created by the wound and the intensity of inflammation.
- Remodeling of connective tissue
- These steps maturation and organization of connective tissue that produces a stable fibrous scar. Wound strength increases due to cross-linking of collagen and increased size of collagen fibers. In addition, there is a shift of the type of collagen deposited, from type III collagen early in repair and to more resilient (flexible) type I collagen
Cutaneous wound healing
- Primary healing/healing by the first intention
- Secondary healing/ healing by second intention
Primary healing/healing by the first intention
Healing of clean, uninfected surgical incision approximated by surgical sutures referred to as primary healing or healing by the first intention. Sequences of events in primary wound healing/ healing by the first intention are following
- Blood clot formation
- Granulation tissue formation
- Cell proliferation and collagen deposition
- Scar formation
- Wound contraction
- Recovery of strength
Healing by first intention (cutaneous wound)
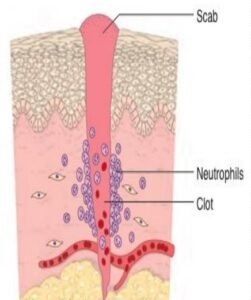
- Formation of a blood clot(within 24 hours)
- Rapid activation of coagulation pathways results in the formation of blood clots and neutrophils appear at the margin of the incision. They release proteolytic enzymes that clean out debris and bacteria and the formation of scab that covers the wound.
- Granulation tissue formation(3-7 days)
- Fibroblasts & vascular endothelial cells proliferate which is called granulation tissue which invades the incision space. By the time 5-7 days, granulation tissue fills the wound area and maximal neovascularization occurs.
- Cell proliferation and collagen deposition occur in 3- 5th days
- Neutrophils replaced by macrophages (by 48-96 hours) and that promote fibroblastic proliferation, angiogenesis, and extracellular matrix deposition, collagen fibers bridge the incision and the epithelial cells proliferate and fuse beneath the surface scab. The epidermis recovers its normal thickness and architecture of the wound.
- Scar formation (Weeks to month)
- Continue accumulation of fibro collagenous tissue. The disappearance of leukocyte infiltrate and edema. -Formation of the scar by connective tissue
Secondary healing/healing by second intention
Healing by secondary intention/ secondary healing occurs when cell or tissue loss is more extensive, ulceration, ischemic necrosis(infarction) in parenchymal organs, and the repair is more complex and involves a combination of regeneration as well as scarring. The secondary healing or healing by the second incision differs from primary healing in the followings:
- Larger tissue defects generate a larger fibrin clot and that fills the defective area (hematoma formation), and the inflammatory reaction is more intense and the granulation tissue formation is more.
- The wound contraction is more by the action of the myofibroblast and scar formation occurs.
Factors affecting wound healing
- Systemic factors
- Nutrition: Protein & vitamin C deficiency and some trace elements such as copper and zinc deficiency – inhibit collagen synthesis and impairs wound healing.
- Age: Wound healing is rapid in young age people compared to in aged people.
- Metabolic states: e.g. Diabetes mellitus is associated with delayed wound healing due to microangiopathy.
- Circulatory status: inadequate blood supply (e.g. arteriosclerosis) or venous abnormalities (e.g. varicose veins) that retard venous drainage and that impairs wound healing.
- Hormones: steroids have anti-inflammatory effects and inhibit collagen synthesis, thereby inhibits wound healing.
- Hematological abnormalities: qualitative or quantitative defects in neutrophils and bleeding abnormalities may delay the healing process.
- Local factors
- Infection: cause delay wound healing.
- Mechanical factor: movement impairs wound healing. E.g: at joints
- Size, location, and type of wound:
- Highly vascularized areas (in a face) heal faster than those in the poorly vascularized area(in feet) small incisional injuries heal faster than large excisional wounds
- Foreign bodies: inessential sutures or foreign bodies (fragments of steel, glass), or even bone can delay the wound healing.
- Ionizing radiation may decrease the repair process.
- Complications may delay wound healing.
The complication of wound healing
- Deficient scar formation
- Excessive formation of the repair components
- Formation of contracture
- Others
- Epidermal cysts
- Pigmentation
- Infection of the wound by different microbes
- Neoplasia: e.g. Squamous cell carcinoma (SCC) may develop in Marjolin’s ulcer.
- Fibrosis: excessive deposition of ECM and collagen.
Defective scar formation
- Inadequate formation of granulation tissue or assembly of scar formation can lead to three complications occur, they are
- Wound dehiscence
- Dehiscence or rupture of the wound is most common after abdominal surgery due to increased abdominal pressure or abdominal distension. It is may occur due to mechanical stress on the abdominal wall: e.g. vomiting and coughing or ileus.
- Ulceration
- Ulceration occurs due to inadequate blood supply during the healing process: for example peripheral vascular disease
- Incisional hernia
- An incisional hernia occurs due to insufficient deposition of the extracellular matrix or inadequate cross-linking in the collagen matrix.
- Wound dehiscence
Excessive formation of the repair component
- Hypertrophied scar: Accumulation of excessive amounts of collagen
- Exuberant granulation: formation of an excessive amount of granulation of tissue that protrudes above the skin surface level. E.g.
- Pyogenic granuloma or granuloma pyogenicum or proud flesh
- Desmoid or aggressive fibromatoses: usually occurs in the anterior abdominal wall.
- Keloid
- If the tissue scar grows beyond the boundaries of the original wound and doesn’t regress so it is called a keloid. (excessive ECM production or excessive deposition of type III collagen) and more common in dark-skinned persons.
- Contraction
- Exaggeration of contraction at the wound site is called contracture resulting in deformities of a wound and surrounding tissues. E.g. in burns
- Site of contracture: Palm, sole and anterior aspect of the thorax.
- Consequences of contractures:
- Compromise movements: burns and joint movements.
- Obstruction: e.g. stricture