What is infarction?
Infarction is the process of formation of an infarct as a result of tissue ischemia. The infarct is a localized area of ischemic necrosis caused by the occlusion of the vascular supply to the affected tissue. Mostly infarct is a coagulative type of necrosis due to sudden occlusion of arterial blood supply. If the patient lives (survives), the infarct size heals with a scar.
Types of infarcts
- Based on color
- Red (hemorrhagic) infarct
- White (anemic) infarct
- Based on age
- Recent or fresh infarct
- Old or healed infarct
- Based on the presence or absence of the infection
- Bland-when it is free of infection.
- Septic-when it is infected.
Pathogenesis of the infarction
- Ischemia is irreversible injury and cell death.
- Necrosis leads to the formation of an infarct.
- Inflammatory response at the periphery
- Repair
- Damaged tissue replaced by scar
- Dystrophic calcification may occur in dead tissue.
Morphology infarction
Gross
- Wedge-shaped infarct
- An occluded vessel at the apex and organ periphery/surface forming the wide base.
- Margins of
- Acute- irregular (poorly defined) and slightly hemorrhagic
- Later- well defined with a rim of hyperemia due to inflammation.
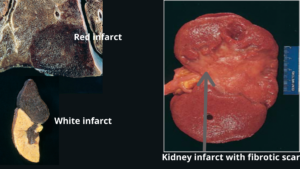
- Red infarcts (hemorrhagic)
- Seen in different conditions:
- Venous occlusion e.g. ovarian torsion
- Loose tissues e.g. lungs
- Tissues with dual blood supply e.g. lungs
- Congested tissues
- Reperfusion of tissue
- Late phase- red blood cells are phagocytosed by macrophages, formation of hemosiderin pigments- firm brown color to tissue.
- Appear as a sharply circumscribed area of necrosis and firm in consistency and dark red to purple in color.
- Seen in different conditions:
- White infarcts (pale or anemic)
- Seen in solid organs with end arterial circulations of the body (e.g. heart, kidney).
- Wedge-shaped with the occluded vessel at the apex and periphery forming the base.
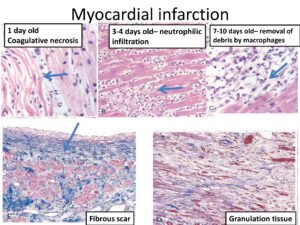
Microscopy
- Ischemic coagulative type of necrosis is most common but liquefactive necrosis in the brain.
- Within 1-2 days: acute inflammatory cells along the margins.
- Infiltration of macrophages – removal of necrotic debris.
- In tissues composed of labile or stable cells, parenchymal regeneration at the periphery of the infarct if stromal architecture is preserved.
- Granulation tissue formation but may replace the infarcted area which matures to form a scar.
- Mostly infarct is replaced by scar.
- Septic infarction: abscess formation.
Factors determining the effects of ischemia and the development of infarct
- Anatomy of the vascular supply
- End arterial circulation- e.g. kidney ( increased the risk of infarction)
- Dual or parallel blood supply- e.g. liver, lungs- decrease chances of infarction
- Rate of occlusion- slow occlusion- time for collaterals development and less chance of infarction
- Tissue vulnerability to ischemia
- E.g. neurons are highly sensitive to hypoxia and undergo necrosis ad damaged within 3 to 4 minutes of ischemia.
- Myocardial cells are quite sensitive to hypoxia but less sensitive than neurons and cells damaged after 20 to 30 minutes.
- Cardiovascular status of an individual – hypoxemia, chronic heart failure increased the risk of infarction.
[embeddoc url=”https://notesmed.com/wp-content/uploads/2021/05/Infarction.pdf” download=”all” cache=”off” text=”complete notes-Download”]