What is the parotid gland?
The parotid (para = around, otic = ear) gland is the largest out of the 3 pairs of salivary glands, viz. parotid gland, submandibular, and sublingual. It is composed almost completely of serous alveoli. The parotid gland is lobulated, yellowish-brown, and weighs about 25 grams.
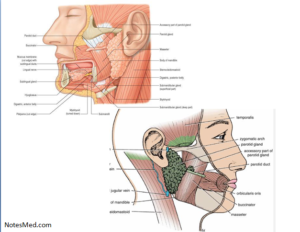
Location: This gland situated in the pyramidal fossa, posterior to the ramus of the mandible which is called the retromandibular fossa (parotid bed).
Boundaries of the Parotid Bed;
- Anteriorly: It is bounded by the posterior border of the ramus of the mandible.
- Posteriorly: It is bounded by the mastoid process.
- Superiorly: It is bounded by the external acoustic meatus & posterior part of the temporomandibular joint (TMJ).
- Medially: It is bounded by the styloid process.
The parotid bed is lined by muscles under the following structures such as;
- Ramus of the mandible: masseter muscle laterally and the medial pterygoid muscle medially.
- Mastoid process: sternocleidomastoid (SCM) muscle laterally and posterior belly of digastric muscle medially.
- Styloid process: styloglossus muscle, stylopharyngeus, and stylohyoid muscle.
Extent
The parotid gland being a soft gland is not confined only to the parotid bed but extends behind it. It extends from,
- Above: External auditory meatus.
- Below: The superior part of the carotid triangle.
- Medially: It extends or elongates to the styloid process (which is closed to the sidewall of the pharynx) & encircle around the neck region of the mandible.
- Posteriorly: It overlaps the sternocleidomastoid(SCM) muscle
- Anteriorly: It extends or elongates over the masseter muscle for a variable distance.
A part of this forward extension is often separated from the rest of the gland and is called the accessory parotid gland. The accessory parotid gland situated between the zygomatic arch above and the parotid duct below. Several ducts are present from the accessory gland open into the parotid duct of the gland.
Parotid capsule/parotid sheath:
The parotid gland is enclosed or surrounded by a fibrous capsule which is known as a parotid capsule. It is composed of the tough investing layer of deep cervical fascia.
The fascia breaks into the region between the angle of the mandible and the mastoid process to enclose the gland in the human.
The superficial lamina is thick, tough, Inflexible, and adherent to the gland while the deep lamina is thin. The superficial lamina combines with the epimysium of masseter to form a thick parotid masseteric fascia, which is attached above to the zygomatic arch in the body.
A thin or narrow deep lamina that is attached to the tympanic plate and styloid process of the temporal bone; thickens to form the stylomandibular ligament of the body, which separates or differentiates the parotid gland from the submandibular gland.
External features
The parotid gland is a three-sided pyramidal shaped with the apex directed downwards. There are the following features shown below;
- An apex.
- Four surfaces:
- Superior surface or base.
- Superficial surface.
- Anteromedial surface.
- Posteromedial surface.
- Three borders:
- Anterior border.
- Posterior border.
- Medial border.
Relations
Apex:
It projects downwards and overlapping the posterior belly of the digastric muscle & adjoining part of the carotid triangle in the human. The structures that come out through the apex include:
- Cervical branches of the facial nerve.
- Anterior and posterior divisions of the retromandibular vein
Superior Surface or Base:
It is concave which is related to the external acoustic meatus and posterior aspect of the temporomandibular joint (TMJ). The following structures that come out through it:
- Superficial temporal vessels.
- Auriculotemporal nerve.
- The temporal branch of the facial nerve.
Superficial Surface:
It is the largest surface out of the four surfaces and covered by the following structures:
- Skin.
- Superficial fascia contains anterior branches of the greater auricular nerve, superficial parotid (preauricular) lymph nodes, and platysma muscle in the body.
- Parotid fascia.
- Deep parotid lymph nodes
Anteromedial Surface:
It is deeply grooved by the posterior border of the ramus of the mandible and is related to the following structures listed below;
- Masseter.
- Medial pterygoid.
- The posterior border (edges) of the ramus of the mandible.
- Lateral aspect of the temporomandibular joint (TMJ).
- Comes out the branches of the facial nerve.
Posteromedial Surface:
It is formed onto the mastoid & styloid processes and their covering muscles and which is related to the following structures:
- Mastoid process, sternocleidomastoid muscle, and posterior belly of the digastric muscle.
- Styloid process and a styloid group of muscles.
The structures that enter the gland through this surface are following:
- Facial nerve trunk in its superior part.
- The external carotid artery in its inferior part.
Anterior Border:
It differentiates the superficial surface from the anteromedial surface. They are the following structures that come out through this border listed below;
- The temporal branch of the facial nerve in the body.
- Zygomatic branch of the facial nerve.
- Transverse facial vessels.
- Superior and inferior buccal branch of the facial nerve.
- Parotid duct.
- The marginal mandibular branch of the parotid duct facial nerve in the body.
Posterior Border:
It separates or differentiates the superficial surface from the posteromedial surface. There are the following structures emerge in this border:
- Posterior auricular vessels.
- Posterior auricular branch of the facial nerve.
Medial Border:
It is also called a pharyngeal border. It separates or differentiates the anteromedial surface from the posteromedial surface. It is associated with the lateral wall of the pharynx.
Structures present within the parotid gland:
The main structures (from superficial to deep) are the following:
- Facial nerve and its branches.
- Retromandibular vein.
- External carotid artery.
- Deep parotid lymph nodes (some members)
- Filaments of the auriculotemporal nerve.
The parotid duct (Stenson’s Duct)
It is about 5 cm in length and 3 mm in width and comes out from the middle of the anterior border of the parotid gland and which opens into the vestibule of the mouth opposite side of the crown part of the upper second molar tooth.
Course:
After coming out from the gland, it runs forward over and above the masseter muscle between the upper and lowers buccal branches of the facial nerve; at the anterior border of the masseter, it suddenly turns inwards, almost at 90° (first bend occur), and penetrates the buccal pad of fat, buccopharyngeal fascia, and buccinator muscle.
After penetrating the buccinator muscle, the parotid duct runs forwards (which is a second bend) for about 1 cm between it and the buccal mucosa.
Finally, the duct turns medially which is the third bend, and opens into the vestibule of the mouth opposite side of the crown part of the upper second molar teeth in the human.
Nerve supply of the parotid gland
Parasympathetic (secretomotor) supply:
- It is supplied through the auriculotemporal nerve. The preganglionic nerve fibers are which is arising from the inferior salivatory nucleus in the medulla and pass immediately one after another through the glossopharyngeal nerve, the tympanic branch of the glossopharyngeal (which is called Jacobson’s nerve), tympanic plexus and lesser petrosal nerve to relay into the otic ganglion.
- Postganglionic nerve fibers are arising from the cells of the ganglion and pass via. the auriculotemporal nerve to provides the parotid gland in the body.
The stimulation of the parasympathetic nerve supply produces a watery secretion in the body.
Sympathetic supply:
- It is obtained from the sympathetic plexus around the external carotid artery which is formed by postganglionic nerve fibers derived from the superior cervical sympathetic ganglion.
- It is preganglionic sympathetic nerve fibers that arise from the lateral horn of the T1 spinal segment. The sympathetic nerve fibers are vasomotor activity and their stimulation produces a thick sticky secretion in your body.
Sensory supply:
- Auriculotemporal nerve.
- Great auricular nerve (C2 and C3).
Blood supply of the parotid gland
- Arterial supply: External carotid and superficial temporal arteries.
- Venous drainage: Retromandibular and external jugular veins.
Lymphatic drainage:
First superficial and deep parotid lymph nodes, which in turn drain into following deep cervical lymph nodes.
Applied anatomy
- The swelling of the parotid gland is very painful due to the fact that inflexible nature of the superficial lamella of the fascial capsule.
- Parotid abscess –It is drained by Hilton’s method to avoid the bruise of branches of the facial nerve.
- Frey’s syndrome: It is a stimulus deliberated for saliva production that produces sweat secretion instead.
[embeddoc url=”https://notesmed.com/wp-content/uploads/2020/09/Parotid-Region.pdf” download=”all”]