What is Yellow fever?
Yellow fever is a zoonotic disease caused by an arbovirus. The yellow fever virus is mostly found in tropical as well as subtropical areas of Africa, Central & South America.
The virus majorly affects monkeys and other vertebrates including human beings. And it is spread to people by the bite of a certain type of infected culicine mosquitoes such as Aedes or Haemagogus species.
This fever is a very rare cause of illness in United States visitors. Illness of yellow fever varies from a mild fever with aches and pains to severe liver damage with bleeding and yellowing skin or sclera (jaundice).
The infection of yellow fever is diagnosed on the basis of their laboratory testing, symptoms of a person, and travel history. Exactly, there is no medicine present to treat or cure an infection.
But to prevent getting sick from yellow fever, use insect resistance, wear long-sleeved shirts and long pants, and get vaccinated early.
The causative agent is Flavivirus fibricus (group B arbovirus, is a member of the togavirus family).
It shares group-specific antigens with other members of the genus like West Nile, dengue, st. Louis encephalitis, and Japanese encephalitis viruses.
Naturally, the virus is pantropic (covers tropical regions of both hemispheres) but after continuous tissue culture as in chick embryo, it loses all its pathogenic properties but retains its antigenicity.
Pathogenesis
The virus is initially introduced to the human body by a mosquito through the skin and spreads to the local lymph nodes where it multiplies.
From the lymph node, it then passes to blood circulation and localizes in the body organ such as liver, spleen, kidney, bone marrow, and lymph glands for several days.
The lesions seen in yellow fever are due to the localization as well as propagation of the virus in a particular area of the organ. Infections may lead to necrotic lesions in the liver and kidney and people die from hepatic and renal damage.
Morphology
The liver shows mid-zonal cloudy and fatty degeneration with necrosis. The necrosed cells now coalesce and become hyalinized which leads to the formation of eosinophilic masses known as Councilman bodies.
In the early stages, acidophilic intranuclear inclusion bodies can be seen in the infected hepatocytes known as Torres bodies.
Symptoms, Diagnosis, & Treatment
According to the CDC, and their studies show that the majority of the population infected with the yellow fever virus will either not have any symptoms, or have mild symptoms and completely recover.
When people develop symptoms, the time from infection up to illness (incubation period) is usually 3 to 6 days.
Due to the fact that there is a risk of severe disease, all people who develop signs and symptoms of yellow fever after traveling to or living in an area at high risk for the yellow fever virus should see their doctors.
Once you have been infected, you are likely to be protected from their future infections.
Symptoms of Yellow fever
Most people will not have any symptoms but when symptoms appear in your body then consult your doctor or healthcare provider.
Some people will develop yellow fever illness with initial symptoms are following;
- Fever of acute onset
- Chills
- Severe headache
- Nausea and vomiting
- Slow pulse
- Back pain
- General body ache
- Fatigue (feeling tired)
- Weakness
- According to the CDC, most people who have initial symptoms improve within one week, with normal treatment or without treatment.
- For some people who recover, weakness and fatigue might last several months to a year.
- Severe symptoms include:
- High fever
- Yellow skin (jaundice)
- Epistaxis (nose bleeding)
- Bleeding and black vomiting
- Melena (bloody stool)
- Shock
- Agitation
- Stupor and coma
- Organ failure
- Severe yellow fever disease can be deadly. If you develop any of these signs and symptoms, see a doctor or consultant immediately and consult about how to manage it.
- Among those who develop severe disease, 30-80% die within the 5th and 10th day of illness due to organ failure (hepatic or renal failure).
- Survivors exhibit life-long immunity so second attacks are unknown. Infants born of immune mothers have antibodies up to 6 months of their life.
Diagnosis
When you and your family are infected with Yellow fever then your doctors are diagnosed on the basis of laboratory testing, symptoms of the person, and travel history.
In laboratory testing includes PCR test, Rapid diagnostic kit, etc. The blood test that looks for viruses or antibodies that a person’s immune system makes against the viral infection.
Treatment of Yellow fever
There is no specific treatment found for yellow fever. Only we can give supportive care to treat dehydration and fever. Associated bacterial infections may be treated with antibiotics.
Supportive care improves outcomes for seriously ill patients.
- No exact medicine to treat or cure an infection of fever.
- Take more rest, drink more fluids, and use pain relievers (reduce fever and pain)
- Maintenance of fluids and electrolytes in your body
- Avoid some specific medications, such as aspirin or other nonsteroidal anti-inflammatory drugs (NSAIDs), for example, ibuprofen (like Advil, Motrin), or naproxen (Aleve), which may increase the risk of bleeding.
- When you have severe symptoms of yellow fever, an infection should need to be hospitalized for close observation and supportive care.
- If after returning from travel you have symptoms of yellow fever (usually about a week), protect yourself from mosquito bites for up to 7 days after symptoms start.
This will help to prevent spreading yellow fever to uninfected culicine mosquitoes that can spread the virus to other people in your family and others.
Modes of transmission
There are 3 known cycles of transmission on the basis of the geographical area involved.
Sylvatic (or jungle) yellow fever
Mainly in tropical rainforests, yellow fever occurs in non-human primates such as monkeys that are infected by wild mosquitoes. The infected monkeys then pass the virus to other normal mosquitoes that feed on them.
The infected culicine mosquitoes bite humans entering the forest, resulting in occasional cases of yellow fever. So, the majority of infections occur in young men visiting or working in the forest (e.g. for logging).
Intermediate (savannah) yellow fever
Mainly in humid or semi-humid parts of Africa, small-scale epidemics occur. Semi-domestic mosquitoes (that breed in the wild environment but around households) infect both monkeys as well as humans.
An outbreak can become a more severe epidemic if the infection is carried into an area populated with both domestic mosquitoes and unvaccinated people.
In this cycle, the virus can be transmitted from monkey to human beings or from human to human via mosquitoes.
Urban yellow fever
Large epidemics may occur when infected people introduce the virus into densely populated areas with a high number of non-immune people and Aedes mosquitoes. Infected mosquitoes can transmit viruses from person to person.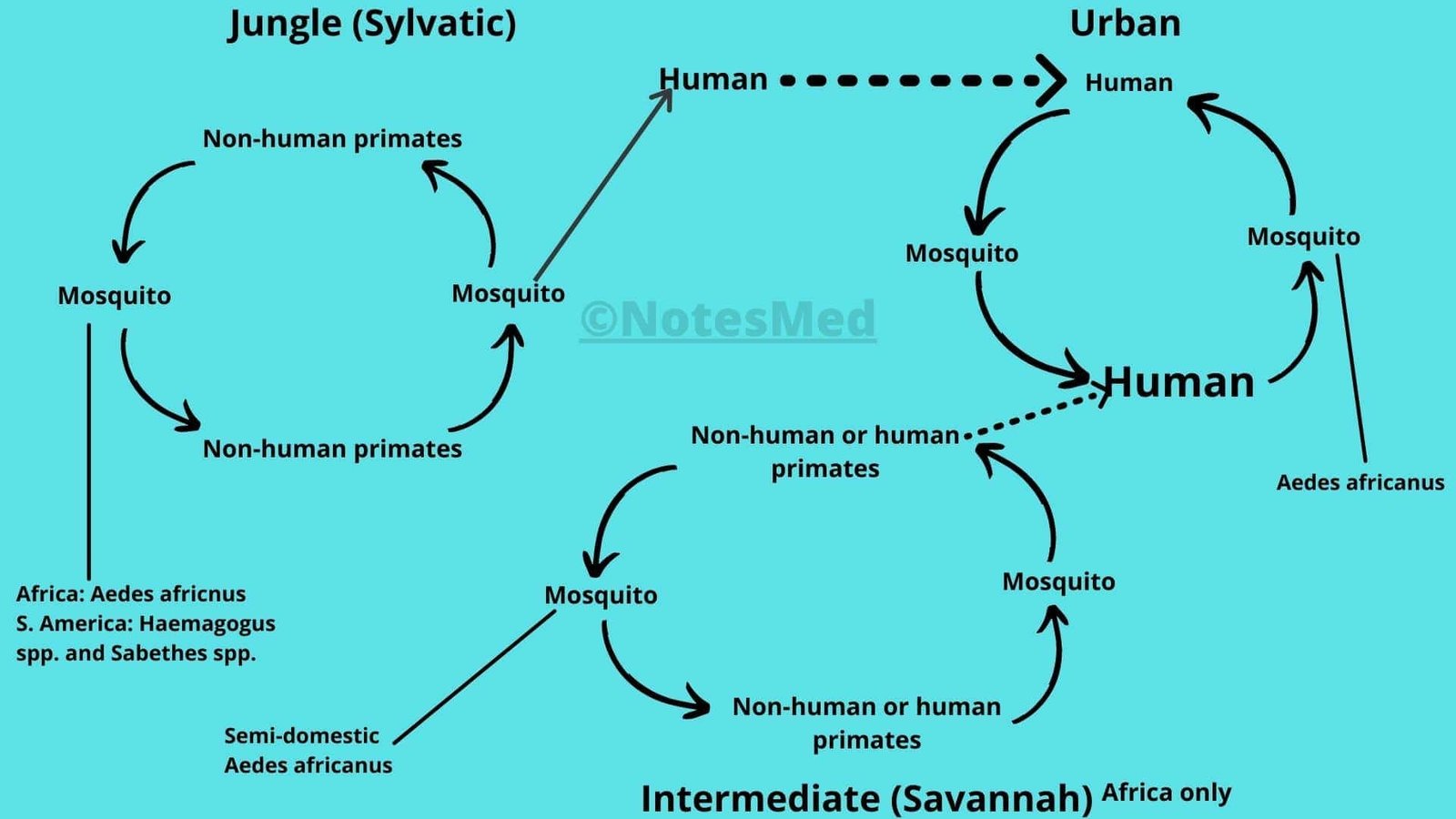
Prevention & Control
Vector control
One of the principal methods of preventing yellow fever is via intensive vector control. The objective is to reduce vector population to the lowest as soon as possible, to stop or reduce quick transmission.
The vector i.e. The Aedes mosquito is peri-domestic inhabits so, can be controlled by anti-adult and anti-larval measures.
It can be done by “source reduction” methods like the elimination of breeding places also, health education.
Personal protection from contact with insects is a major factor in integrated vector control.
The measures include the use of insect repellents (like Oil of lemon eucalyptus, para-menthane-diol, 2-undecanoate, etc), mosquito nets, mosquito coils, and fumigation mats, wear long-sleeved shirts and long pants, etc.
Surveillance
Program of surveillance (like clinical, serological, histopathological and entomological, etc.) should be carried out in endemic areas for the early detection of virus in human populations or in animals that may contribute to its dissemination.
For the surveillance program of Aedes mosquitoes, the WHO uses an index known as the Aedes aegypti index.
This is defined as “the percentage of houses and their premises, in a limited well-defined area, showing actual breeding of Aedes aegypti larvae.
This index should be < 1 percent in towns and seaports (endemic areas) to ensure freedom from yellow fever.
Vaccination
A single dose safe and effective yellow fever vaccine provides lifelong protection for most people.
In general, the Yellow fever vaccine is recommended for people who are 9 months old or older and who are traveling to or living in areas at risk for the yellow fever virus in Africa, Central & South America.
There are two very effective vaccines that have been developed for human use.
French Neurotropic Vaccine (Dakar)
This is produced from the infected mouse brain and used. This vaccine carries a greater risk of producing encephalitis in the vaccines, especially in children. And it was later replaced by a vaccine called the non-neurotropic (17D) vaccine.
17D Vaccine
This is a safe and equally effective vaccine as Dakar. This vaccine was developed by Theiler in 1937 bypassing the Asibi strain serially in the mouse embryo and whole chick embryo tissues.
And then after in chick embryo tissue from which the central nervous tissue has been removed and this has been used as a vaccine for > 40 years.
This vaccine is thermolabile and is administered by subcutaneous inoculation. Immunity develops within 10 days of vaccination.
Vaccine recommendations
After Vaccination, some people may have the chance to develop an allergic reaction to the vaccine, but may still benefit from being vaccinated.
These people, or their parents, should talk and consult your doctor or consultant as soon as possible.
- Between 6 and 8 months old child
- Over 60 years old people
- Pregnant women
- Breastfeeding women
In few conditions, people should not get the vaccine. There are the following conditions:
- People who are allergic to a vaccine
- Aged 6 months or younger child
- Organ transplant recipients people
- Diagnosed with a cancerous (malignant) tumor in the people
- Diagnosed with a disorder of the thymus gland & associated with the abnormal immune system and its function
- Diagnosed with primary immunodeficiency disorder.
- Using immunosuppressive and immunomodulatory therapies in human beings.
- Symptoms are seen in HIV-infected persons or CD4+ T-lymphocytes less than 200/mm3.
Yellow Fever Vaccine, Pregnancy, & Conception
The vaccine has been given to most pregnant women without any obvious adverse effects on the fetus. However, since the yellow fever vaccine is a live vaccine, it poses various theoretical risks.
Pregnant women should evade or postpone travel to an area where there is a high risk of yellow fever. If travel cannot be evaded, discuss or consult vaccination with your doctor or consultant.
While a 2-week delay between vaccination of yellow fever and conception is almost certainly sufficient, a one-month delay has been recommended as a more conservative approach.
If for some reason behind, a woman is vaccinated during the pregnancy period, she is unlikely to have some problems from the vaccine but her baby is very probable to be born healthy.
Frequently Asked Questions
- What is yellow fever?
- Where does the yellow fever virus occur?
- Who found the real cause of yellow fevers?⇒Walter Reed discovered and studied yellow fever and Max Theiler first developed a yellow fever vaccine.
- How before long individuals become ill in the wake of being nibbled by a contaminated mosquito?
- What are the symptoms and causes of yellow fevers?
- How are yellow fevers diagnosed?
- Are yellow fevers still around today?
- Are yellow fevers life-threatening?
- What is the treatment for yellow fever?
- What stopped yellow fevers?
- How long did yellow fevers last?
- How can people lessen the chance of getting infected with the yellow fever virus?
- How would it be a good idea for me to respond in the event that I figure a relative may have yellow fevers?
- I just received the yellow fever vaccine. Do I have to keep away from contact with my immunocompromised relatives?
No, there is no evidence that people who receive vaccines shed the vaccine virus. Therefore, there is no need to avoid people, including those whose immune systems do not work well.
- Who should get or not get the yellow fever vaccine?
- How long does yellow fevers vaccination last?
- Will I have to go to a particular clinic to get a yellow fever vaccination?
- Is the yellow fever vaccine recommended for people 60 years and older who will be traveling to areas with a risk of yellow fevers?
- What are the possible side effects of vaccination?
- I think I became ill from the immunization, how would it be advisable for me to respond?
- Does the vaccine contain thimerosal?⇒No.
- How long should a lady stand by to imagine subsequent to getting a yellow fevers immunization?
- Could Yellow Fever be passed from one individual to another and how to spreads?
- Was yellow fever a pandemic?
- Which portion of the body do yellow fevers assault?