What is Treponema pallidum?
Treponema pallidum is a causative agent of an ancient sexually transmitted disease called ‘syphilis’. The name pallidum refers to its pale-staining property.
Morphology of Treponema pallidum
Treponemes are very thin and delicate with tapering ends. Size varies (6- 14 μm x 0.2 μm). Spirals: Flexible, spirally coiled around an axis; posses 6-14 spirals spaced at intervals of 1 μm with an amplitude of 1-1.5 μm.
Motility: Actively motile exhibiting flexion-extension, translatory, and corkscrew motility. Thye have a typical tendency to bend at a right angle at the midpoint.
Endoflagella: Around 3-4 flagella are present in this periplasmic space that helping in tissue invasion & dissemination. They are also extremely antigenic, stimulating a strong early antibody response.
Treponemes cannot be visualized by a light microscope but can be seen under dark ground or a phase-contrast microscope. They do not take up ordinary stain but can be stained by fluorescence staining and silver impregnation method (increase the thickness of bacilli).
Types of syphilis
Primary syphilis
Primary (or hard) chancre:
- It is a single painless papule that is rapidly becoming ulcerated, hard, and indurated.
- The most common sites are the penis in the case of males), the cervix or labia in the case of females, and the anal canal, rectum, or mouth in homosexuals.
Regional (usually inguinal) lymphadenopathy:
- Appear within 1 week of onset of skin lesions.
- The painless firm, non-suppurative, and often bilateral lymph node.
- The chancre normally heals within 4-6 weeks (range is about 2- 12 weeks), but lymphadenopathy may persist for months.
Non-venereal mode:
- If transmitted by direct contact→ the primary chancre is extragenital, generally on the fingers.
- If transmitted by blood transfusion → the primary chancre does not appear.
Secondary Syphilis
Usually develops 4-8 weeks after the healing of the primary lesions. Skin and mucous membranes are commonly affected & it may be characterized by
- Skin rashes (palms and soles).
- Condylomata lata.
- Mucous patches (superficial mucosal erosions).
- Generalized lymphadenopathy.
Latent syphilis
- After secondary lesions disappear, subclinical. It may persist for years. Diagnosis by serological tests.
- Early latent syphilis’s initial time period is 4-years and late latent period.
- Early latency: relapses and is infectious.
Tertiary or late-stage
- A decade or so after tertiary lesions: gamma or granulomatous nodules (skin, mucous membrane, bone, tongue, liver, testes, aorta, myocardium).
- Cardiovascular syphilis: aortitis, aortic aneurysm, aortic incompetence, and coronary ostial stenosis.
- Neurosyphilis: tabes dorsalis, general paralysis of insane (GPI), and meningovascular syphilis may develop and not common (except neurosyphilis in HIV patients).
Congenital syphilis
- Usually from primary and secondary infection.
- Untreated: About 40% fetal loss due to stillbirth, prematurity, and neonatal death, etc.
Survivor:
- Half is asymptomatic (seropositive) and the remainder similar to secondary syphilis.
- Late manifestations: after 2 years.
Nonvenereal syphilis
Non-venereal syphilis is similar to venereal except extra-genital chancre. It is rarely by transfusion of infected blood.
Laboratory diagnosis of Treponema pallidum (syphilis)
Specimen:
Fluid or scrapings from:
- Chancre (primary stage).
- Mucous patches and condyloma (secondary stage, congenital syphilis).
Tissue biopsy.
DIRECT DEMONSTRATION:
Dark-ground microscopy:
- Slender, spiral organism present on the microscope exhibiting rotational as well as flexion and extension movements.
- Stained smear: DFA-TP, silver impregnation method
- PCR: Most sensitive, commercially not available.
SEROLOGICAL TESTS:
Non-specific reagin antibody:
- It is most useful as screening (standard test for syphilis).
Specific anti-treponemal antibody –confirmatory test.
NON-SPECIFIC(NONTREPONEMAL) TESTS:
Antibodies produced to a tissue lipoidal material (reagin).
Cardiolipin antigen is known as ‘standards tests for syphilis’ (STS). First STS: Wasserman complement fixation test (not in use).
Flocculation tests:
- Tube flocculation test: Kahn test
- Slide test: VDRL simpler and more rapid.
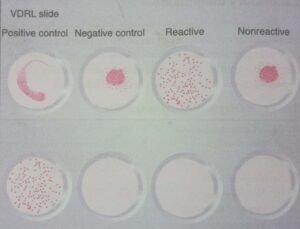
VENEREAL DISEASE RESEARCH LABORATORY (VDRL):
Most widely used. VDRL antigen (cardiolipin) must be prepared fresh daily. Specially prepared glass slide with depression of about 14 mm diameter each. 0.05 ml decomplemented serum. A single drop of freshly prepared cardiolipin antigen is added on & rotate at 180 rpm for 4 minutes.
Observed under a microscope:
- Negative result: uniformly distributed cardiolipin crystals.
- Positive reaction: the presence of clumps.
In the positive case, should perform quantitative tests. It is not highly specific.
Good screening test: 99% sensitivity in secondary syphilis. It can be done with CSF but it cannot be used for testing plasma.
Automated VDRL-ELISA test.
MODIFIED VDRL TESTS:
Modifications,
- Rapid plasma reagin(RPR) test.
- Unheated serum reagin(USR) test.
- Toluidine red unheated serum test (TRUST).
Rapid plasma reagin(RPR) test:
It is similar to the VDRL test and finely divided carbon (charcoal) particles and choline are added to stabilized VDRL antigen. It can be read visually snd can be performed with unheated serum or plasma. It is not recommended for testing cerebrospinal fluid. It is an easier and more specific screening test than the VDRL test.
Advantages of RPR:
- Commercially available.
- Unheated serum.
- Can be read visually.
- A finger-prick blood is sufficient.
- Either plasma (EDTA blood) or serum can be used
Disadvantage:
- Cannot be used with CSF.
Biological false-positive tests:
- The major disadvantage of STS. Especially in the low prevalence of syphilis but is useful for screening.
- Titre of BFP: rarely exceeds 1:8 an incidence less than 2%.
- BFP antibody is mainly IgM.
- In syphilis: mainly IgG.
Acute BFP:
- Viral diseases (measles, infectious mononucleosis), mycoplasma pneumonia, malaria, and following certain vaccinations.
Chronic BFP reaction:
- Leprosy, in 10-20% of patients with autoimmune diseases (SLE, polyarteritis nodosa, rheumatic disorder), and in intravenous drug users.
Treponemal tests:
2 types: Group-specific and species-specific.
- Group-specific:
-
- For avoiding BFP.
- Lipopolysaccharide-protein complex antigen derived from Reiter treponemes and it is not in use nowadays.
Species-specific (treponemal antibody) test:
- Treponema pallidum as antigen (live, killed, or extract of virulent Nichol’s strain).
- Treponema pallidum immobilization (TPI) test.
- Fluorescent treponemal antibody absorption test (FTA-ABS)
- Treponemal pallidum particle agglutination(TP-PA) test
- Micro-haemagglution assay MHA-TP) test.
Treponema pallidum immobilization(TPI) test:
- It is actively motile Nichol’s strain of T. pallidum.
- Immobilized in presence of specific antibodies.
Fluorescent treponemal antibody absorption test (FTA-ABS:
- It is an indirect fluorescent antibody test.
Micro-haemagglution assay MHA-TP) test:
- It is sensitized red cells are mixed with the patient’s serum, cells clump together.
Treponemal pallidum particle agglutination(TP-PA) test:
- It is Sensitized gelatin particles are mixed patient’s serum particles agglutinate in positive cases.
Enzyme-immunoassay (EIA):
- It is an ideal screening test for mass surveys. Sensitivity and specificity about 90 & 98% respectively.
Diagnosis of congenital syphilis:
T. pallidum in skin lesions or in CSF.
Specific IgM anti treponemal antibodies.
Treatment:
- DOC: penicillin –Never shown to produce β-lactamase.
- Tetracycline or doxycycline.
[embeddoc url=”https://notesmed.com/wp-content/uploads/2020/08/Treponema-pallidum.pdf” download=”all” cache=”off”]