What is temporomandibular joint (TMJ)
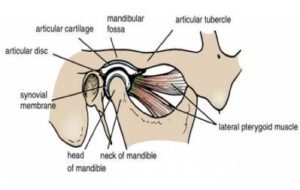
The temporomandibular joint (TMJ) is a synovial joint of condylar variety between temporal bone and mandible that allows the movements of the mandible for speech and mastication present on each side of the head.
The temporomandibular joint (TMJ) is a synovial joint of condylar variety between temporal bone and mandible that allows the movements of the mandible for speech and mastication present on each side of the head.
Articular surface
- The upper articular surface is formed by the articular fossa and articular eminence of the temporal bone.
- The lower articular surface is formed by the head or condyle of the mandible.
- And the articular surface is covered by fibrocartilage but not by hyaline cartilage, hence the joint is an atypical synovial joint present in the human being.
The joint cavity of Temporomandibular Joint
The joint cavity is subdivided completely by the articular disc into the menisco-temporal and lower menisco-mandibular compartment.
Ligament of the Temporomandibular Joint
- Capsular ligament with synovial membrane
- Articular disc
- Lateral or temporo-mandibular ligament
- Accessary ligaments- spheno-mandibular & stylomandibular ligaments
Capsular ligament
Attachment of the capsule:
- Above- articular tubercle Infront, squamotympanic fissure behind & peripheral margin of the mandibular fossa in between them.
- Below – around the neck of the mandible
- In front – combined with the insertion of lateral pterygoid.
- The inner surface of the capsule is firmly circumference to the peripheral margin of the articular disc.
- Above the disc, the capsule is loose & below the disc it is taut. The synovial membrane lines the inside of the capsule of the joint but does not extend to cover the disc or the articular surfaces.
Articular disc
It is an oval plate of fibrocartilage that caps the head of the mandible & divides the joint completely into 2 compartments.
A thick margin forms the peripheral annulus and central depression on the lower surface. From before backward, the upper surface of the concavo-convex disc.
Posteriorly, the disc splits into upper & lower lamellae by a venous plexus and the upper lamella is attached to squamo- tympanic fissure & the lower lamella is attached to the posterior surface of the mandible of the neck.
Parts of the articular disc
- From before backward
- Anterior extension
- Anterior thick band
- Intermediate zone
- Posterior thick band
- Posterior bilaminar zone
Lateral or temporo-mandibular ligament
The lateral ligament is a true ligament and formed as a result of thickening on the lateral aspect of the capsular ligament.
The attachment is above the articular tubercle on the root of the zygomatic process of the temporal bone.
It extends downwards and backward at an angle of 45° to the horizontal, to attach to the lateral surface and posterior border of the neck of the condyle.
Sphenomandibular ligament
The sphenomandibular ligament descends from the spine of the sphenoid to reach the lingula of the mandibular foramen.
This part is a vestige of the dorsal end of Meckel’s cartilage and the relations of the Sphenomandibular ligament are following laterally; lateral pterygoid muscle, auriculo-temporal nerve, maxillary artery, and inferior alveolar nerve and vessels.
And the medially related with medial pterygoid, chorda tympani nerve, and wall of the pharynx.
The clinical correlation of the Sphenomandibular ligament is an important landmark for the administration of the local anesthetic during inferior alveolar nerve block.
Stylomandibular ligament
The stylomandibular ligament is formed by condensation of deep cervical fascia and extends from the tip of the styloid process to the angle of the mandible. It divides the parotid gland from the submandibular gland.
Relations In Temporomandibular Joint
- Lateral
- Skin and fasciae.
- Parotid gland.
- Temporal branches of the facial nerve.
- Medial
- Tympanic plate separating it from the internal carotid artery.
- The spine of the sphenoid.
- Auriculotemporal nerve.
- Middle meningeal artery.
- Sphenomandibular ligament.
- Chorda tympani nerve.
- Anterior
- Tendon of lateral pterygoid.
- Masseteric nerve and vessels.
- Posterior
- Postglenoid part of the parotid gland separating it from the external auditory meatus.
- Superficial temporal vessels.
- Auriculotemporal nerve
- Blood supply-By the superficial temporal and maxillary vessels.
- Nerve supply – By the auriculotemporal and masseteric branches of the mandibular nerve.
- Lymphatic drainage: by the superficial parotid (preauricular) nodes, deep parotid nodes, upper deep cervical nodes.
Movements of Temporomandibular Joint
There are various movements are shown in TMJ such as elevation, depression, protrusion, retraction & side to side movement.
The range of movement in the maximal opening of the mouth is 50-60 mm. The mandible may be protruded or laterally displaced 10 mm.
- Side to side movement:
- It takes place in chewing and the lateral & medial pterygoid muscle of one side acting alternately with the other side.
- The chin moves in the side where rotation has occurred and gliding movement occurs on the opposite side.
- Protrudes: lateral and medial pterygoids have a major role in this type of movement.
- Retractors: posterior fibers of temporalis assisted by fibers of the masseter, digastric, and geniohyoid involved in these movements.
- Elevators: anterior and middle fibers of temporalis, superficial and deep fibers of the masseter, and medial pterygoid are involved.
- Depressors: lateral pterygoids aided by digastric, geniohyoid, and mylohyoid are involved.
- Lateral movement: medial and lateral pterygoids muscles of each side.
Applied anatomy
Temporomandibular joint syndrome / internal derangement
It is a group of symptoms arising from the temporomandibular joints and their associated masticatory muscles.
In this case, spread facial pain due to masseteric muscle spasm, headache because of the temporalis muscle spasm, and jaw aches due to lateral pterygoid spasm are typical presenting symptoms.
These may be associated with clicking, which is often audible whilst the patient is chewing, and sometimes locking when the patient is unable to open fully.
TMJ dislocation
In this condition, the mandibular head is displaced from the articular tubercle in the infratemporal fossa by a sudden spasm of lateral pterygoid muscle during the wide opening of the mouth as yawning.
Reduction of dislocation
The condyle must be lowered and pushed back behind the summit of the articular eminence into the articular fossa.
Muscles of Mastication
There are four principal muscles are involved in mastication, they are:
- Temporalis muscle
- Masseter muscle
- Lateral pterygoid muscle
- Medial pterygoid muscle
TMJ movements are produced principally by the muscles of mastication. They develop from the mesoderm of the embryonic first pharyngeal arch. Consequently, they are all innervated by the nerve of that arch, the(motor root of the) mandibular nerve (CN V3).
Origin and insertion of muscles
[embeddoc url=”https://notesmed.com/wp-content/uploads/2021/05/Temporomandibular-Joints.pdf” download=”all” text=”Complete pdf file-Download”]