What are parathyroid glands?
The parathyroid glands are small yellowish-brown in color bodies. It is ovoid or lentiform in shape glands & about 6 mm long in its greater diameter, 3 mm breadth, and 2 mm thickness glands.
It is about 0.4 gram mass of parathyroid gland in the body. Generally, four in number present on the posterior border of the thyroid gland, which is lying within its fascial capsule in the glands.
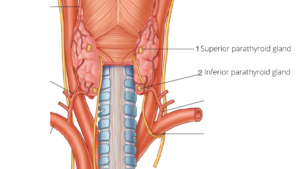
These glands lie at the middle of the posterior border of the thyroid lobe above the level at which the inferior thyroid artery crosses the recurrent laryngeal nerve and these glands develop from the 4th pharyngeal pouch and hence also called parathyroid-IV.
The position of these superior parathyroid glands more constant than the inferior ones.
-
Inferior parathyroid glands:
The glands lie on the posterior border of the thyroid lobe near its lower pole (inferior pole), below the inferior thyroid artery.
These glands may lie:
- Within the thyroid capsule, under the loop of the inferior thyroid artery
- Outside the capsule, above the loop of the thyroid artery, or
- Within the substance of the thyroid gland.
These glands develop from the 3rd pharyngeal pouch, hence also called parathyroid-III.
Blood supply
- The superior parathyroid artery:
It is supplied to the superior parathyroid glands.
It is a branch from the anastomotic artery joining the superior and the inferior thyroid arteries, or from the inferior thyroid artery.
- The inferior parathyroid artery:
It is supplied to the inferior parathyroid glands and the inferior parathyroid artery is a good guide to locate the parathyroid gland especially if it lies below the thyroid gland.
Nerve supply
It is supplied by the sympathetic fibers, derived from the superior and middle cervical sympathetic ganglia or sympathetic plexus around the inferior thyroid artery and these fibers are vasomotor in nature.
Micro-Anatomy (Histology)
- Connective tissue capsule that sent septa into the gland.
- The parenchyma of the gland contains two types of cells i.e. Chief cells or principal cells, and oxyphil cells.
-
- Chief cells:
It is small polygonal cells that are pale staining, slightly acidophilic cytoplasm. The chief cells have granules containing the parathyroid hormone. - Oxyphil cells:
- It is larger polygonal cells that are acidophilic cytoplasm and their function is not known.
- Chief cells:
The parathyroid hormone increases the number and activity of osteoclasts.
Development
- Superior parathyroid glands: It develops from the endodermal part of the 4th pharyngeal pouch.
- Inferior parathyroid gland: It is developed from the endoderm part of the 3rd pharyngeal pouch.
Applied anatomy
- Hyperparathyroidism:
- In this condition decrease phosphate levels in the blood and an increase in blood calcium level.
It is seen in the tumors of the parathyroid glands and the increased amount of parathormone;
- Removes excessive calcium compounds from bones, which makes the bones soft because of decalcification leading to cause generalized osteitis fibrosa, and it may cause the formation of kidney stones in the body.
- In this condition decrease phosphate levels in the blood and an increase in blood calcium level.
- Hypoparathyroidism:
- In this clinical condition increased blood phosphate level and decreased blood calcium level.
- Denser and more mineralized bones that lead to cause spastic contraction of skeletal muscles is called tetany due to exaggerated excitability due to lack of calcium level in blood.