What is benign prostatic hyperplasia?
Benign prostatic hyperplasia is the enlargement of the prostate glands resulting from the proliferation of stromal and glandular elements. It is the most common benign prostatic disease in men >50 years and the frequency rises progressively reaching 90% by 80 years.
The most common area is transitional and periurethral zones of the prostate gland. The large nodules compress & narrow the urethral canal to cause various symptoms.
Pathophysiology of benign prostatic hyperplasia:
Dihydrotestosterone (DHT) is produced after testosterone is acted by the enzyme type 2 5α-reductase. Dihydrotestosterone (DHT) is 10 times more potent. The 5α-reductase is located in stromal cells.
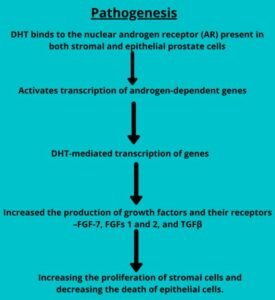
- The dihydrotestosterone (DHT) binds to the nuclear androgen receptor (AR) present in both stromal and epithelial prostate cells.
- Then activates transcription of androgen-dependent genes.
- The dihydrotestosterone (DHT)-mediated transcription of genes and increased the production of growth factors and their receptors-FGF-7, FGFs 1 and 2, and TGFβ.
- Stromal proliferation increases and decreasing the death of epithelial cells.
Morphology of benign prostatic hyperplasia
Gross:
- Weighs between 60 and 100 gm. The site is the inner aspect of the prostate gland which is the transition zone.
- Cross-section:
- Nodules: vary in color and consistency.
- If mostly glands: yellow-pink with a soft consistency.
- If mostly fibromuscular stroma: pale gray and tough.
- Microcystic areas and the urethra: compressed into a slit-like lumen.
Microscopy:
- The hallmark of benign prostatic hyperplasia is nodularity. The nodules range from purely stromal fibromuscular nodules to fibroepithelial nodules with a glandular predominance.
- In the glands:
- Proliferation with aggregations of small to large to cystically dilated glands.
- It is lined by two layers, an inner columnar and an outer cuboidal or flattened epithelium.
- Papillary infoldings of the glands.
Clinical features:
- Increased urinary frequency.
- Nocturia.
- Difficulty in starting & stopping the passes of urine.
- Overflow dribbling.
- Dysuria (painful micturition).
Complications:
- Bacterial infections of bladder and kidney.
- Acute urinary retention.
Diagnosis:
- Digital rectal examination: A finger inserts into the rectum to check the prostate for enlargement.
- Transrectal ultrasound
- Prostate-specific antigen blood test: prostate-specific antigen (PSA) is a substance produced in the prostate. PSA levels increase when the prostate enlarged. However, elevated PSA levels can also be due to recent procedures, infection, surgery, or prostate cancer, etc.
Treatments:
The best choice of treatment depends on various factors, including:
- The size of the prostate.
- Age
- Overall health is yours.
- The amount of discomfort or bother you are experiencing in the infectious time.
Medication:
The medication is the most common treatment for mild to moderate symptoms of prostate gland enlargement. There are following options include:
- Alpha-blockers: Dilates and relax bladder neck muscles and muscle fibers in the prostate, making urination easier. e.g. alfuzosin, doxazosin, tamsulosin and silodosin.
- 5-alpha reductase inhibitors: It inhibits enzyme type 5α-reductase and prevents the formation of dihydrotestosterone. e.g. finasteride and dutasteride.